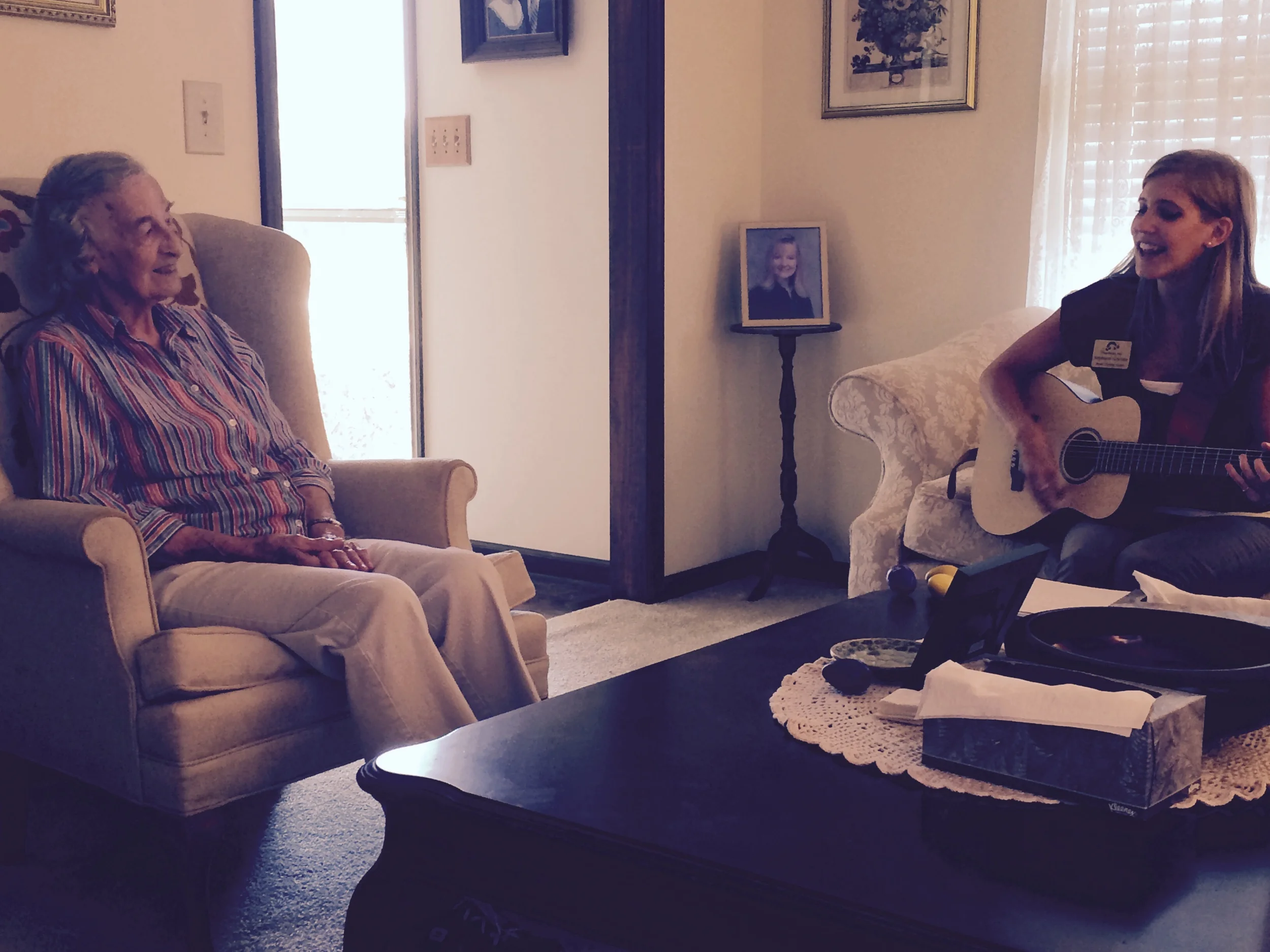
Even though this internship is focused on kids being that it is a pediatric center, Perry and I have the wonderful opportunity to see one very special geriatric client. She has been diagnosed with Alzheimer’s disease and is in the early to middle stages. Though she likes to think she is already 90 years old, this sweet 89-year-old lady welcomes us each week and loves singing along to the familiar music we present to her. She may not remember who we are each week, or that she has repeated the same couple of sentences 3 times already, but she does remember the lyrics to old songs she grew up hearing. Why is that?
This topic of music on the effects of Alzheimer’s disease has been and continues to be studied by researchers all around the world. Over recent years, stories have been hitting the news about the positive effects music has on elderly patients with dementia and Alzheimer’s. A story Atlanta Alive did on music therapy in memory units of nursing homes brought tears to a news anchor because, he describes, it’s an eye-opening experience seeing how beneficial music therapy is in bringing these patients momentarily out of their confusion and back into good times of the past.
Researchers in a 2014 study titled, The Role of Singing Familiar Songs in Encouraging Conversation Among People with Middle to Late Stage Alzheimer’s Disease report that this neurodegenerative disease causes the loss of more than just memory and cognition. It affects communication both expressively and receptively, making it troublesome for these patients to speak fluidly, spontaneously, or purposefully and thus can produce social isolation (Dassa & Amir, 2014).
While our client is still capable of producing speech, it is upon arriving to her house that we can usually hear her humming and making nonsensical vocalizations to herself, filling the silence. It seems that she craves music and dialogue, and we have the privilege of providing that for her!
Two weeks ago, I sang “Battle Hymn of the Republic” with the very catchy “Glory, glory, hallelujah” refrain. She kind of nodded along, but did not sing along much at all. Just last week, I presented the song again and she sang along every time that refrain came up, with enthusiasm! She even sang parts of the verses too. She seemed more present and moved her feet along to the beat. Did the repetition of the song spark an uplifting memory within her? Connie Tomaino, a well-renowned music therapist who works mainly with individuals who have suffered from stroke, other brain injury, and neurodegenerative diseases, states that the structural form of music (melody, lyrics) is not the only thing people remember about familiar songs, but that these songs also elicit memories and “rich associations” related to the song. Listening or singing along to these memorable tunes can bring to the forefront a sense of self that may have gotten lost through the progressive disease (Tomaino, 2002). Oliver Sacks, neurologist and author of Musicophilia: Tales of Music and the Brain, calls music a “memory aid that elicits long-forgotten emotions and associations, giving the patient access to moods, memories, and thoughts” (Sacks, 2008).
It is well known that individuals with Alzheimer’s have difficulty staying focused and engaged in the topic at hand. Despite this, the researchers found in the aforementioned 2014 study that after singing familiar songs with a group of 65-83-year olds with middle to late stage Alzheimer’s disease twice a week for 4 weeks, the participants were more able to concentrate and take part in the following conversations than they were able to before without music (Dassa & Amir, 2014).
Using music therapy with individuals with Alzheimer’s disease is beneficial in a variety of ways. Participating in singing or playing along to familiar songs allows the client to feel a sense of belonging, a sense of accomplishment; engage in communication, gross and fine motor movements, breath control, relaxation; and of course recall memories associated with the music, which can bring back that sense of self, maintaining their dignity. Dassa & Amir reference a 2009 study concluding that, “in a disease that destroys memory, preserved musical memory could serve as an important tool to enhance the quality of life for people who have lost so many other abilities” (Dassa & Amir, 2014).
It is a joy to watch our client sing along and exercise gross and fine motor movements to the beat of the song. She always expresses her gratitude when we are leaving and asks us to come again! After researching more about music therapy with patients with Alzheimer’s, I now plan on integrating a little more dialogue and open-ended questions into the sessions after the songs to not only engage our client in conversation, but also to assess how much and what kinds of memories and associations the songs evoke in her.
References
Dassa, A., & Amir, D. (2014). The role of singing familiar songs in encouraging conversation among people with middle to late stage Alzheimer’s disease. Journal of Music Therapy, 51(2), 131-153. doi: 10.1093/jmt/thu007.
Sacks, O. (2008). Musicophilia – Tales of music and the brain. New York: Alfred A. Knopf.
Tomaino, C. (2002). The role of music in the rehabilitation of persons with neurologic diseases. Music Therapy Today (online). Retrieved from http://www.wfmt.info/Musictherapyworld